BIRTH CONTROL

DEPO-PROVERA INJECTION
IUD
BIRTH CONTROL IMPLANTS
DIAPHRAGM
TUBAL LIGATION
BIRTH CONTROL PILL (oral contraceptive)
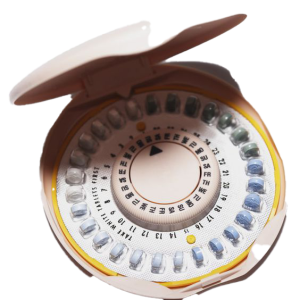 What is “the Pill”?
What is “the Pill”?
Combined oral contraceptives are commonly known as “the pill”. They contain two man-made hormones called estrogen and progestin.
The various brands of pills differ ONLY by the amount of estrogen in each pill and by the type and amounts of progestin. Some pills contain a constant dose of hormones while others are phasic in which the amount of hormones change to mimic your natural menstrual cycle.
Each package contains 21 hormonally active pills followed by 7 placebo pills (28-day regimen) or 7 days of taking no pills (21-day regimen).
How does the Pill work?
The pill prevents ovulation, which is the release of eggs from the ovaries. It also causes thickening of the cervical mucus to block sperm from entering the cervix and affects the lining of the uterus to prevent implantation of the pregnancy.
How effective is the Pill?
Among perfect users (women who miss no pills and follow instructions perfectly), only about 1 in 1000 women will become pregnant over the first year of use. Among typical users, about 3 to 5 in 100 women will become pregnant over one year of use. Pregnancy rates during typical use are based on the number of missed pills and delay in starting the next pill pack.
Am I a good candidate for the Pill?
Most healthy women of reproductive years are good candidates for the pill regardless of prior pregnancy history if interested in birth control and are able to take a pill every day.
This includes teens, overweight or underweight women, diabetics without underlying heart disease, women with family history of breast cancer, women over 35 who are non-smokers, and smokers under 35 (however, it is best NOT to take the pill and smoke!) The pill does NOT protect from sexually transmitted diseases particularly HIV. If this is a concern you should also use a condom.
What are the most common side effects of the Pill?
Many of the side effects from the pill are due to the estrogen component and usually resolve within the first few months of starting the pill. Thus, new pill starters are encouraged to try the pill for at least 3 months.
Nausea
Caused by the estrogen component. Try taking the pill at night or with a snack. You may benefit from starting with the lowest estrogen dose (20 mcg) pill.
Breast tenderness
Both the estrogen and progestin components of the pill may contribute to breast tenderness. Eliminating caffeine and chocolate from your diet may help.
Menstrual changes
Breakthrough bleeding or any irregular bleeding may occur within the first 3 months of use, especially if you have missed pills or are not taking them at the same time each day. Breakthrough bleeding does not decrease the effectiveness of thepill provided you are taking them daily. If this persists after 3 months, often a change to a higher dose pill or simply a different brand will help. If intermenstrual bleeding persists, you may need to be checked for other causes of bleeding unrelated to pill use.
Headache
If you develop headaches while on the pill, these need to be evaluated by your doctor. If you suffer from any neurological symptoms such as changes in vision or tingling/numbness in your extremities then you should immediately discontinue the pill as estrogen will increase your risk of stroke. If headaches continue or worsen without neurological complaints, you may want to switch to the lowest dose estrogen pill or simply a different formulation. Women who suffer from menstrual migraines usually benefit from being on the pill.
Hypertension
The pill may cause an increase in blood pressure in some women. New users should have their pressure checked 3 months after starting the pill and all women should have it checked at each doctor’s visit. Women with a known history of hypertension that is well-controlled on medications may be able to take the pill but should consult with their primary care doctor.
Gallbladder disease
The pill may stimulate the growth of gallstones in women with existing gallbladder disease.
What are the benefits of the Pill?
-
- more regular and predictable menses
- decrease in the number of days of bleeding and amount of blood loss each month
- decrease in menstrual cramps
- decreases acne (all brands decrease testosterone which decreases acne)
- improves hirsutism (excessive hair growth)
- decreases benign breast disease (fibroadenoma and cystic changes)
- lifetime decrease risk of ovarian cancer by 40% continuing at least 15 years after use
- lifetime decrease risk of endometrial cancer by 50%
- decreased risk of colorectal cancer in current users and within 10 years of use
- desirable effect on cholesterol; increases the good cholesterol while decreasing the bad cholesterol
- preserves bone density and possible reduction in osteoporosis
When do I start the Pill?
You must wait for your next period to ensure that you are NOT pregnant when you start the pill. You can start EITHER:
Day-1 start: on the first day of bleeding
Sunday start: on the Sunday following the first day of bleeding.
If you start the pill on a Sunday, you will NOT get your period on the weekend. If you start the pill within the first five days of your period you will be protected from pregnancy that first month and not need a back-up method.
You can use the following regimen to benefit from a Sunday Start and still have immediate protection from pregnancy. If your period starts on a Monday or Tuesday, this regimen will shorten your cycle by one or two days, which is not harmful to you. Then start your next and all subsequent pill packs on the Sunday following completion of the prior pack.
How do I take the Pill?
You must take one (active) pill every day. Most packs contain 3 weeks of hormonally active pills followed by one week of inactive pills (or 7 days of taking no pills) during which time you will get your period. The placebo pills serve as a reminder to get you into the habit of taking a pill every day and not forgetting to start your next pack. Try linking it to something you do the same time every day (i.e. brushing your teeth before going to bed).
What If I miss a Pill?
If you miss any of the inactive pills throw out all pills missed. If you miss any of the hormonally active pills:
Missed 1 pill in any week. Take the missed pill NOW and the next pill at the usual time (this may entail taking 2 pills now). You will be protected from pregnancy but may have some breakthrough bleeding or spotting for the remainder of the pill pack. This should resolve when you start your next pack.
Missed 2 pills in week 1 or 2. Take 2 pills NOW and 2 pills tomorrow. Then take 1 pill a day until you finish the pack. Use a backup method of contraception (i.e. condom) for the next 7 days. Again, you may have some bleeding or spotting for the remainder of the pill pack.
Missed 2 pills in week 3 or missed 3 or more pills. For Day-1 Start: Throw out pack. Start new pack the same day. Use a backup method for 7 days. For Sunday Start: Take 1 pill each day until Sunday. On Sunday, throw out the old pack and start a new pack. Use a backup method for 7 days.
If you do miss 2 or more pills and are concerned you may be pregnant, emergency contraception or the “morning-after pill” is available. This must be taken within 72 hours (or 3 days) of unprotected intercourse. You may call the office to receive this form of contraception. Please note that the morning after pill is only intended for occasional use and not as a regular method of birth control.
Are there any warning signs I should look out for once I start the Pill?
Call your doctor if you have any of the following problems: severe abdominal pain; severe chest pain (shortness of breath or sharp pain on breathing); severe headache, dizziness, weakness or numbness, especially if one sided; eye problems (vision loss or blurring), speech problems; or severe calf or thigh pain.
Which Pill is right for me?
There is no exact formula to determine which particular pill is best for you-every woman responds differently to different pills. Despite advertising, essentially all oral contraceptives work equivalently well.
For you, the best pill is the one with the least amount of estrogen that does the job. In addition to protecting, you from pregnancy, the pill should regulate your periods and some women do need more estrogen for this purpose.
Price is another consideration. Most pills are $25-$35 or more per month. Many health insurance prescription plans do not cover birth control pills. The more popular, better-advertised pills can be more expensive. There are equally effective and appropriate pills for you that are less expensive.
There are also programs available, such as femScript, that subsidize the cost of the pill. Ask about these alternatives.
Are there any reasons why I shouldn’t use the Pill?A woman should not use the pill if she has history of:
- Stroke or other diseases of the blood vessels
- Blood clots in the lungs or legs
- Heart attack
- Active liver disease
- Migraine headaches with changes in vision or tingling/numbness in the extremities
- Age over 35 years and a smoker
- Current or past history of breast cancer
DEPO-PROVERA INJECTION
 What is “the Injection”?
What is “the Injection”?
Depo-Provera is a progestin-only injectable form of birth control given by your health care provider every 3 months. It is injected into either your upper arm or buttocks. The next injection should be scheduled in 12 weeks-this gives you a week or two of flexibility if you are unable to keep that appointment.
How does the Injection work?
It prevents pregnancy by stopping ovulation (the release of an egg from the ovary). It thickens the mucus around the cervix preventing sperm from entering the cervix and alters the lining of the womb to inhibit implantation of the pregnancy.
How effective is the Injection?
Depo-Provera is more than 99% effective. Of every 1,000 women who use this method, 3 will become pregnant during first year of use. This is one of the most effective forms of birth control.
Am I a good candidate for the Injection?
Depo-Provera is worth considering if you want long-term contraception without following a daily routine. Since protection is maintained from a injection every 3 months, it allows for sexual spontaneity. It may also be a good choice for you if you cannot remember take a pill every day or if you cannot use birth control containing estrogen (i.e. you are over 35 and a smoker or have a history of blood clots.) It is also a good choice if you do NOT plan to become pregnant in the near future and want a reliable form of birth control other than the pill.
The injection does not protect from sexually transmitted diseases particularly HIV. If this is a concern you should use a condom as well.
Are there any reasons why I shouldn’t use the Injection?
Most women who need birth control can use Depo-Provera, regardless of age. * A woman should not use the injection if she has history of:
- Active liver disease
- Current or past history of breast cancer
- Unexplained vaginal bleeding* The final decision is between you and your doctor.
What are the common side effects of the Injection?
Irregular bleeding
Almost all women who use Depo-Provera will experience changes in their period, including irregular or unpredictable bleeding or spotting, and occasionally heavy or continuous bleeding. This tends to subside the longer you use this method. After a year of use, one-half of women will stop having a period altogether. This is an expected side effect from the injection and is NOT a medical problem. The constant release of hormone in your body from the injection prevents the lining of the uterus from building up; therefore, there is nothing to bleed off each month. If the irregular bleeding is interfering with your lifestyle, talk to your health care provider. This condition can be treated by either taking a short course of estrogen (i.e., taking the birth control pill) or medications such as Motrin or Advil to regulate your cycle for a few months until the irregular bleeding resolves.
Weight gain
Depo-Provera has been shown to be associated with weight gain. As much as 3 to 5 lbs. in the first year of use. This is most likely due to increased appetite from the progestin. If you watch what you eat and exercise regularly you can offset this weight gain.
Delay in the return of your period
Although the injection does NOT cause infertility, it may take 12 to18 months from your last injection for your normal menstrual function to return (the average is 10 months). Thus, if you are considering pregnancy in the near future you may want to consider an alternative method of birth control.
No immediate discontinuation
Unlike, the pill or mini pill, the hormone given as an injection can take several months to clear from your body. Thus, you may be “stuck” with some of the other side effects such as irregular bleeding, weight gain, etc. for several months.
Reversible loss of bone mass
Women who use Depo-Provera for a long period of time may have lower density than non-users. This will reverse after stopping the Depo-Provera and has not been shown to cause osteoporosis or associated fractures. Women over 40 who continue this method for greater than 2 years would benefit from having their bone density checked.
Mood changes
Some women experience mood changes on the injection-depression, irritability, and change in sex drive. These are infrequent side effects.
What are the benefits of the Injection?
Easy to use–all you have to remember is to go to your health care provider for a injection 4 times a year
Extremely reliable–this form of birth control has one of the lowest failure rates
Confidential–no one other than your health care provider needs to know you are using it decreases menstrual cramps and blood loss–after 1 year of use 50% of women will no longer get their period
Reversible–although expect a delay in the return of your period of 10 months on average
When can I start taking the Injection?
We will only give you the Depo-Provera within 5 days of the start of your menstrual period. This ensures that you are NOT pregnant when you receive the injection and it will be effective immediately. Before you get each injection, we will check that you have a negative urine pregnancy test.
Another time to start this method is after the end of a pregnancy; either at the time of termination of pregnancy or within 5 days postpartum if NOT breastfeeding. If you plan to breastfeed, Depo-Provera is a safe method of birth control, but we recommend waiting until 6 weeks postpartum when the milk supply is fully established. If you initiate Depo-Provera after the birth of a child, keep in mind the delay in return of your menstrual cycle. If you are planning to have another baby within the next year or so, you may want to select a different form of birth control.
What If I am late for my next Injection?
If you are late for your Depo-Provera, we want to make sure that you are NOT pregnant. However, now we need to do a blood pregnancy test to make sure you are not pregnant. This is much more sensitive test than a urine test. The blood test usually takes one day for results. If negative, you could return the next day for your injection but you should use condoms as a backup method for the next two weeks.
Are there some warning signs I should look out for once I start the Injection?
- Call your doctor if you have any of the following problems:
- Repeated, very painful headaches
- Heavy bleeding (soaking more than one menstrual pad per hour)
- Depression
- Pus, prolonged pain, or bleeding at injection site severe lower abdominal pain
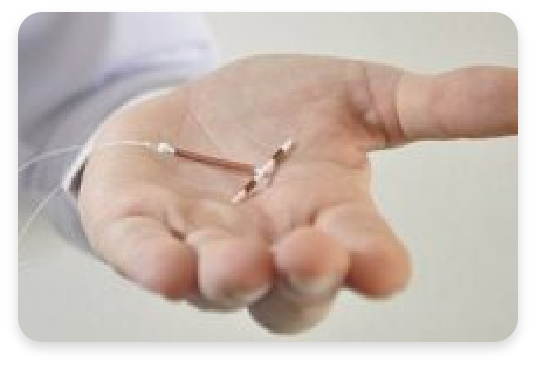
IUD (intrauterine contraceptive device)
vaginal barrier contraception
 What is the IUD?
What is the IUD?
The IUD is a small, plastic device that is inserted by a physician / practitioner and left inside the uterus. Although there have been several types of IUDs, currently only two are available in the United States.
Both are T-shaped and have a string at the base of the T that will extend through the cervix and lie in the vaginal canal. The copper IUD releases a small amount of copper into the uterus and may remain in your body for up to 10 years. The hormonal IUD releases a small amount of the hormone progesterone into the uterus, but must be replaced every year.
How does the copper IUD work?
It primarily prevents pregnancy by interfering with the movement of sperm thus preventing fertilization of the egg. The copper IUD prevents fertilization as well as affecting the lining of the uterus so implantation will not occur.
How effective is the copper IUD?
The IUD is extremely effective. During the first year of use, 8 out of 1000 women will become pregnant with the Copper T.
Am I a good candidate for the copper IUD?
The copper IUD is best suited for women with families who want convenient, effective, reversible contraception. It is recommended for women who have at least one child, are in a stable, mutually faithful relationship (to minimize chance of exposure to sexually transmitted diseases that might cause pelvic inflammatory disease) and have no history or suspicion of pelvic infection.
Are there any reasons why I shouldn’t use the copper IUD?
For some women, certain conditions can increase the chance of having problems with the IUD. The IUD may NOT be a good choice if you have:
- had a pelvic infection
- had an ectopic (tubal) pregnancy
- severe pain during menstrual periods
- abnormal vaginal bleeding
- multiple sexual partners or a high risk for sexually transmitted diseases
- allergy to copper
What are the common side effects of the copper IUD?
Irregular bleeding
Bleeding problems constitute one of the more common IUD complications. Some women have cramping and spotting during the first few weeks after the IUD is placed. These should disappear within a month. The IUD does cause slightly crampier and longer menstrual periods. These symptoms can be treated with Motrin or Advil.
Pelvic infection
The risk of developing a pelvic infection associated with the IUD is attributable to insertion of the device and exposure to sexually transmitted infection. The greatest risk occurs during the first few weeks following insertion. Women who have more than one sexual partner or whose partner has other sexual partners are at high risk for acquiring a sexually transmitted disease.
Expulsion
Between 2 and 10% of IUD users spontaneously expel their IUD within the first year. Expulsion, though infrequent, is more likely to occur during the first 3 months of use. An IUD expulsion can occur without a woman knowing it. Therefore, you should check regularly to make sure the “string” is still present.
What are the benefits of the copper IUD?
- Highly effective
- Easy to use
You don’t have to remember to insert it before sex or take a pill every day.
Reversible
It can be easily removed in the office if you decide to get pregnant and you do not need to wait before attempting pregnancy.
Can be used by breastfeeding women
There is no affect on lactation.
Inexpensive
After the first year of use, the annual cost for using the IUD is less expensive per year.
May be used by women who cannot use hormonal methods and causes no systemic side effects
(except in women allergic to copper or have a condition called Wilson’s disease)
Comfort
You should not be aware of the presence of the IUD. You and your partner should not be able to feel the IUD during intercourse.
When can the copper IUD be inserted?
First it must be determined that you are a good candidate for the IUD. Your doctor will take a medical history, perform a pelvic exam and obtain any appropriate lab tests.
The insertion can then be scheduled within the first 5 days of your next menstrual period; this insures that you are not pregnant at the time of insertion and the method is effective immediately for birth control.
The IUD can also be placed after giving birth, as soon as your uterus has returned to its normal pre-pregnancy state. It can be determined whether you are ready for IUD insertion at your postpartum check.
How is the copper IUD inserted?
You may be given some antibiotics to take prior to insertion to protect from infection. Also, taking 3-4 Motrin or Advil an hour prior to insertion will minimize the discomfort of the insertion.
Insertion of the IUD does not require anesthesia. Immediately before the IUD is inserted, you will be asked to sign a consent form making sure you understand everything about the insertion and a pregnancy test will be checked.
To insert the IUD, the arms of the T-shaped device are folded and the IUD is placed in a long, slender, plastic tube. The tube is then inserted into the vagina and guided through the cervix into the uterus. The IUD is then pushed out of the plastic tube into the uterus and the tube is withdrawn.
Each IUD comes with a string or “tail” made of a thin plastic thread. After insertion the thread is trimmed so that 1-2 inches hang out of the cervix inside your vagina. You will be able to tell about the placement of the IUD by the location of the string. The string will not bother you, but your partner may feel it with his penis.
If you feel discomfort, the string may be further trimmed. It is important that you check the string each month. To do this, you must insert a finger into your vagina and feel around for the string. You can do this at any time, but doing it after your menstrual period is easy to remember. If you feel the string is shorter or longer than it used to be-or if you don’t feel the string at all-call your doctor.
The IUD may have slipped out of place. Use another form of birth control until your IUD is checked.
Are there any warning signs I should look out for after the IUD is inserted?
Call your doctor if you have any of the following problems:
- Severe abdominal pain
- Pain during intercourse
- Bleeding or spotting that occurs between periods, after intercourse, or that lasts more than a few months
- Missed period or other signs of pregnancy
- Unusual vaginal discharge
- A change in length or position of the string
BIRTH CONTROL IMPLANTS
 Birth control implants are devices that go under the skin. A hormone is released that prevents pregnancy.
Birth control implants are devices that go under the skin. A hormone is released that prevents pregnancy.
DIAPHRAGM (vaginal barrier contraception)
 What is the Diaphragm?
What is the Diaphragm?
The diaphragm is a round rubber dome that fits inside a woman’s vagina and covers her cervix. It must be used with spermicide (a sperm-killing cream or jelly).
How does the Diaphragm work?
The diaphragm is a barrier method of birth control that prevents pregnancy by placing a physical and chemical “wall” between the sperm and the cervix. It must always be used with a spermicidal cream or jelly. Be sure that the jelly or cream you purchase is a spermicide containing nonoxynol-9.
How effective is the Diaphragm?
The diaphragm is NOT the most effective form of birth control. Effectiveness includes the use of spermicide. Among perfect users (women who use the diaphragm EVERY time they have sex), about 6 in 100 women (6%) is expected to become pregnant over the first year of use. Among typical users, 18 in 100 women will become pregnant over one year of use. However, using a condom along with the diaphragm will increase the effectiveness AND provide protection from sexually transmitted disease.
Am I a good candidate for the Diaphragm?
The diaphragm is worth considering if you cannot or prefer not to use hormonal birth control. You must be able to use it every time you have sex.
Are there any reasons why I shouldn’t use the Diaphragm?
The diaphragm may not be a good choice for you if you are unlikely to use it correctly every time you have sex. You may not be able to use it if you or your partner is sensitive to the chemicals used in spermicides or has a latex allergy. You may have a higher failure rate if you have intercourse three or more times per week.
What are the most common side effects of the Diaphragm?
- Increased risk of urinary tract infections
- Yeast infections and bacterial vaginosis
- Sensitivity due to latex allergy
What are the benefits of the Diaphragm?
- Almost no side effects and does not affect your hormonal pattern
- Lower risk of cervical cancer and pre-cancerous conditions of the cervix
How do I use a Diaphragm?
Wash your hands carefully with soap and water before inserting the diaphragm. Apply spermicidal cream or jelly around the rim and inside the dome of the diaphragm. You may put spermicide on both sides of the diaphragm, but make certain to apply a generous amount of spermicide on the side of the diaphragm facing or in contact with the cervix.
Squeeze the rim of the diaphragm between your fingers and insert it into your vagina. When the diaphragm is pushed up as far as it will go, the front part of the rim should be up behind a bone you can feel in front of your pelvis (the pubic bone). Tuck the front rim of the diaphragm up as far as it will comfortably go.
Check to see if your cervix is covered. To do this, reach inside and touch your cervix. The cervix feels something like the tip of your nose. After the diaphragm is in place, the cervix should be completely covered by the rubber dome.
When do I insert the Diaphragm?
The diaphragm may be placed up to 6 hours before you have sex. No matter when you insert the diaphragm, always be sure to use a spermicide. Diaphragms should not be used without this added protection.
If you have put in the diaphragm more than 2 hours before having sex, you must insert a fresh supply of spermicide into your vagina just before intercourse. To do this, insert the spermicide with an applicator while the diaphragm is in place. An applicator usually comes with the spermicide.
You must also check the position of the diaphragm and add more spermicide before each act of intercourse, no matter how closely together they occur. Do not use oil-based lubricants such as petroleum jelly; they can damage the diaphragm. Water-based lubricants such as KY jelly or Astroglide are fine.
When should I remove the Diaphragm?
The diaphragm must be left in place for 6 hours after you have sex, but should NOT be worn for more than 24 hours. To remove the diaphragm, pull gently on the front rim. Wash it with mild soap and water, rinse the soap off well (soap can harm the rubber), dry it, and put it back in its case.
When do I need to replace the Diaphragm?
The diaphragm may become discolored over time, but it can still be used unless you notice any holes in the rubber. To check for holes, hold the diaphragm up to the light and stretch the rubber gently between your fingers. Filling the diaphragm with water is another way to check for holes.
You should get a new diaphragm about every 2 years. Your diaphragm should be rechecked at your yearly exam and should be refitted if you have:
- had pelvic surgery
- been recently pregnant
- gained or lost a lot of weight
- trouble with the diaphragm slipping out of place, pain or pressure during sex
What should I do if I forgot to use the Diaphragm or placed it incorrectly?
Emergency contraception is available if you are concerned that may be pregnant. This can only be used within 72 hours of unprotected or inadequately protected intercourse. Call the office to find out more about this back-up method of birth control.
Are there any warning signs I should look out for when using a Diaphragm?
There is a slight increased risk of toxic shock syndrome in diaphragm users if it is worn for more than twenty-four hours.
Call your doctor if you have any of the following problems:
Sudden high fever, vomiting, diarrhea, dizziness, faintness, weakness, sore throat, aching muscles and joints, or a rash (like a sunburn).
BIRTH CONTROL

BIRTH CONTROL (CONTRACEPTION)
There are several different contraception options available ranging from a daily pill to medical procedures that permanently prevent pregnancy.
Our office offers the best and most comprehensive range of birth control options to date in the NYC metropolitan area. Our focus is to help you decide which birth control method will best fit your lifestyle and comfort level.
BIRTH CONTROL PILL (oral contraceptive)
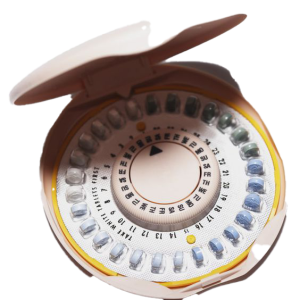
What is “the Pill”?
Combined oral contraceptives are commonly known as “the pill”. They contain two man-made hormones called estrogen and progestin.
The various brands of pills differ ONLY by the amount of estrogen in each pill and by the type and amounts of progestin. Some pills contain a constant dose of hormones while others are phasic in which the amount of hormones change to mimic your natural menstrual cycle.
Each package contains 21 hormonally active pills followed by 7 placebo pills (28-day regimen) or 7 days of taking no pills (21-day regimen).
How does the Pill work?
The pill prevents ovulation, which is the release of eggs from the ovaries. It also causes thickening of the cervical mucus to block sperm from entering the cervix and affects the lining of the uterus to prevent implantation of the pregnancy.
How effective is the Pill?
Among perfect users (women who miss no pills and follow instructions perfectly), only about 1 in 1000 women will become pregnant over the first year of use. Among typical users, about 3 to 5 in 100 women will become pregnant over one year of use. Pregnancy rates during typical use are based on the number of missed pills and delay in starting the next pill pack.
Am I a good candidate for the Pill?
Most healthy women of reproductive years are good candidates for the pill regardless of prior pregnancy history if interested in birth control and are able to take a pill every day.
This includes teens, overweight or underweight women, diabetics without underlying heart disease, women with family history of breast cancer, women over 35 who are non-smokers, and smokers under 35 (however, it is best NOT to take the pill and smoke!) The pill does NOT protect from sexually transmitted diseases particularly HIV. If this is a concern you should also use a condom.
What are the most common side effects of the Pill?
Many of the side effects from the pill are due to the estrogen component and usually resolve within the first few months of starting the pill. Thus, new pill starters are encouraged to try the pill for at least 3 months.
Nausea
Caused by the estrogen component. Try taking the pill at night or with a snack. You may benefit from starting with the lowest estrogen dose (20 mcg) pill.
Breast tenderness
Both the estrogen and progestin components of the pill may contribute to breast tenderness. Eliminating caffeine and chocolate from your diet may help.
Menstrual changes
Breakthrough bleeding or any irregular bleeding may occur within the first 3 months of use, especially if you have missed pills or are not taking them at the same time each day. Breakthrough bleeding does not decrease the effectiveness of thepill provided you are taking them daily. If this persists after 3 months, often a change to a higher dose pill or simply a different brand will help. If intermenstrual bleeding persists, you may need to be checked for other causes of bleeding unrelated to pill use.
Headache
If you develop headaches while on the pill, these need to be evaluated by your doctor. If you suffer from any neurological symptoms such as changes in vision or tingling/numbness in your extremities then you should immediately discontinue the pill as estrogen will increase your risk of stroke. If headaches continue or worsen without neurological complaints, you may want to switch to the lowest dose estrogen pill or simply a different formulation. Women who suffer from menstrual migraines usually benefit from being on the pill.
Hypertension
The pill may cause an increase in blood pressure in some women. New users should have their pressure checked 3 months after starting the pill and all women should have it checked at each doctor’s visit. Women with a known history of hypertension that is well-controlled on medications may be able to take the pill but should consult with their primary care doctor.
Gallbladder disease
The pill may stimulate the growth of gallstones in women with existing gallbladder disease.
What are the benefits of the Pill?
-
- more regular and predictable menses
- decrease in the number of days of bleeding and amount of blood loss each month
- decrease in menstrual cramps
- decreases acne (all brands decrease testosterone which decreases acne)
- improves hirsutism (excessive hair growth)
- decreases benign breast disease (fibroadenoma and cystic changes)
- lifetime decrease risk of ovarian cancer by 40% continuing at least 15 years after use
- lifetime decrease risk of endometrial cancer by 50%
- decreased risk of colorectal cancer in current users and within 10 years of use
- desirable effect on cholesterol; increases the good cholesterol while decreasing the bad cholesterol
- preserves bone density and possible reduction in osteoporosis
When do I start the Pill?
You must wait for your next period to ensure that you are NOT pregnant when you start the pill. You can start EITHER:
Day-1 start: on the first day of bleeding
Sunday start: on the Sunday following the first day of bleeding.
If you start the pill on a Sunday, you will NOT get your period on the weekend. If you start the pill within the first five days of your period you will be protected from pregnancy that first month and not need a back-up method.
You can use the following regimen to benefit from a Sunday Start and still have immediate protection from pregnancy. If your period starts on a Monday or Tuesday, this regimen will shorten your cycle by one or two days, which is not harmful to you. Then start your next and all subsequent pill packs on the Sunday following completion of the prior pack.
How do I take the Pill?
You must take one (active) pill every day. Most packs contain 3 weeks of hormonally active pills followed by one week of inactive pills (or 7 days of taking no pills) during which time you will get your period. The placebo pills serve as a reminder to get you into the habit of taking a pill every day and not forgetting to start your next pack. Try linking it to something you do the same time every day (i.e. brushing your teeth before going to bed).
What If I miss a Pill?
If you miss any of the inactive pills throw out all pills missed. If you miss any of the hormonally active pills:
Missed 1 pill in any week. Take the missed pill NOW and the next pill at the usual time (this may entail taking 2 pills now). You will be protected from pregnancy but may have some breakthrough bleeding or spotting for the remainder of the pill pack. This should resolve when you start your next pack.
Missed 2 pills in week 1 or 2. Take 2 pills NOW and 2 pills tomorrow. Then take 1 pill a day until you finish the pack. Use a backup method of contraception (i.e. condom) for the next 7 days. Again, you may have some bleeding or spotting for the remainder of the pill pack.
Missed 2 pills in week 3 or missed 3 or more pills. For Day-1 Start: Throw out pack. Start new pack the same day. Use a backup method for 7 days. For Sunday Start: Take 1 pill each day until Sunday. On Sunday, throw out the old pack and start a new pack. Use a backup method for 7 days.
If you do miss 2 or more pills and are concerned you may be pregnant, emergency contraception or the “morning-after pill” is available. This must be taken within 72 hours (or 3 days) of unprotected intercourse. You may call the office to receive this form of contraception. Please note that the morning after pill is only intended for occasional use and not as a regular method of birth control.
Are there any warning signs I should look out for once I start the Pill?
Call your doctor if you have any of the following problems: severe abdominal pain; severe chest pain (shortness of breath or sharp pain on breathing); severe headache, dizziness, weakness or numbness, especially if one sided; eye problems (vision loss or blurring), speech problems; or severe calf or thigh pain.
Which Pill is right for me?
There is no exact formula to determine which particular pill is best for you-every woman responds differently to different pills. Despite advertising, essentially all oral contraceptives work equivalently well.
For you, the best pill is the one with the least amount of estrogen that does the job. In addition to protecting, you from pregnancy, the pill should regulate your periods and some women do need more estrogen for this purpose.
Price is another consideration. Most pills are $25-$35 or more per month. Many health insurance prescription plans do not cover birth control pills. The more popular, better-advertised pills can be more expensive. There are equally effective and appropriate pills for you that are less expensive.
There are also programs available, such as femScript, that subsidize the cost of the pill. Ask about these alternatives.
Are there any reasons why I shouldn’t use the Pill?A woman should not use the pill if she has history of:
- Stroke or other diseases of the blood vessels
- Blood clots in the lungs or legs
- Heart attack
- Active liver disease
- Migraine headaches with changes in vision or tingling/numbness in the extremities
- Age over 35 years and a smoker
- Current or past history of breast cancer
DEPO-PROVERA INJECTION
 What is “the Injection”?
What is “the Injection”?
Depo-Provera is a progestin-only injectable form of birth control given by your health care provider every 3 months. It is injected into either your upper arm or buttocks. The next injection should be scheduled in 12 weeks-this gives you a week or two of flexibility if you are unable to keep that appointment.
How does the Injection work?
It prevents pregnancy by stopping ovulation (the release of an egg from the ovary). It thickens the mucus around the cervix preventing sperm from entering the cervix and alters the lining of the womb to inhibit implantation of the pregnancy.
How effective is the Injection?
Depo-Provera is more than 99% effective. Of every 1,000 women who use this method, 3 will become pregnant during first year of use. This is one of the most effective forms of birth control.
Am I a good candidate for the Injection?
Depo-Provera is worth considering if you want long-term contraception without following a daily routine. Since protection is maintained from a injection every 3 months, it allows for sexual spontaneity. It may also be a good choice for you if you cannot remember take a pill every day or if you cannot use birth control containing estrogen (i.e. you are over 35 and a smoker or have a history of blood clots.) It is also a good choice if you do NOT plan to become pregnant in the near future and want a reliable form of birth control other than the pill. The injection does not protect from sexually transmitted diseases particularly HIV. If this is a concern you should use a condom as well.
Are there any reasons why I shouldn’t use the Injection?
Most women who need birth control can use Depo-Provera, regardless of age. * A woman should not use the injection if she has history of:
- Active liver disease
- Current or past history of breast cancer
- Unexplained vaginal bleeding
- * The final decision is between you and your doctor.
What are the common side effects of the Injection?
Irregular bleeding
Almost all women who use Depo-Provera will experience changes in their period, including irregular or unpredictable bleeding or spotting, and occasionally heavy or continuous bleeding. This tends to subside the longer you use this method. After a year of use, one-half of women will stop having a period altogether. This is an expected side effect from the injection and is NOT a medical problem. The constant release of hormone in your body from the injection prevents the lining of the uterus from building up; therefore, there is nothing to bleed off each month. If the irregular bleeding is interfering with your lifestyle, talk to your health care provider. This condition can be treated by either taking a short course of estrogen (i.e., taking the birth control pill) or medications such as Motrin or Advil to regulate your cycle for a few months until the irregular bleeding resolves.
Weight gain
Depo-Provera has been shown to be associated with weight gain. As much as 3 to 5 lbs. in the first year of use. This is most likely due to increased appetite from the progestin. If you watch what you eat and exercise regularly you can offset this weight gain.
Delay in the return of your period
Although the injection does NOT cause infertility, it may take 12 to18 months from your last injection for your normal menstrual function to return (the average is 10 months). Thus, if you are considering pregnancy in the near future you may want to consider an alternative method of birth control.
No immediate discontinuation
Unlike, the pill or mini pill, the hormone given as an injection can take several months to clear from your body. Thus, you may be “stuck” with some of the other side effects such as irregular bleeding, weight gain, etc. for several months.
Reversible loss of bone mass
Women who use Depo-Provera for a long period of time may have lower density than non-users. This will reverse after stopping the Depo-Provera and has not been shown to cause osteoporosis or associated fractures. Women over 40 who continue this method for greater than 2 years would benefit from having their bone density checked.
Mood changes
Some women experience mood changes on the injection-depression, irritability, and change in sex drive. These are infrequent side effects.
What are the benefits of the Injection?
Easy to use–all you have to remember is to go to your health care provider for a injection 4 times a year
Extremely reliable–this form of birth control has one of the lowest failure rates
Confidential–no one other than your health care provider needs to know you are using it decreases menstrual cramps and blood loss–after 1 year of use 50% of women will no longer get their period
Reversible–although expect a delay in the return of your period of 10 months on average
When can I start taking the Injection?
We will only give you the Depo-Provera within 5 days of the start of your menstrual period. This ensures that you are NOT pregnant when you receive the injection and it will be effective immediately. Before you get each injection, we will check that you have a negative urine pregnancy test.
Another time to start this method is after the end of a pregnancy; either at the time of termination of pregnancy or within 5 days postpartum if NOT breastfeeding. If you plan to breastfeed, Depo-Provera is a safe method of birth control, but we recommend waiting until 6 weeks postpartum when the milk supply is fully established. If you initiate Depo-Provera after the birth of a child, keep in mind the delay in return of your menstrual cycle. If you are planning to have another baby within the next year or so, you may want to select a different form of birth control.
What If I am late for my next Injection?
If you are late for your Depo-Provera, we want to make sure that you are NOT pregnant. However, now we need to do a blood pregnancy test to make sure you are not pregnant. This is much more sensitive test than a urine test. The blood test usually takes one day for results. If negative, you could return the next day for your injection but you should use condoms as a backup method for the next two weeks.
Are there some warning signs I should look out for once I start the Injection?
- Call your doctor if you have any of the following problems:
- Repeated, very painful headaches
- Heavy bleeding (soaking more than one menstrual pad per hour)
- Depression
- Pus, prolonged pain, or bleeding at injection site severe lower abdominal pain
IUD (intrauterine contraceptive device)
vaginal barrier contraception
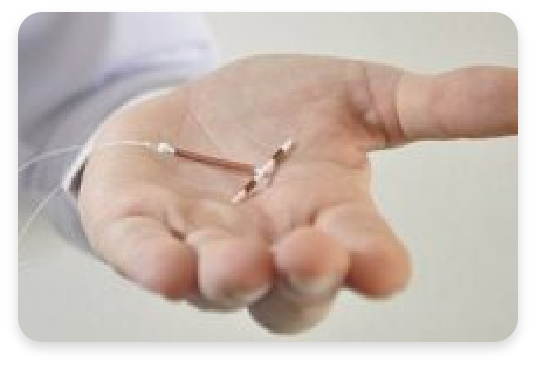 What is the IUD?
What is the IUD?
The IUD is a small, plastic device that is inserted by a physician / practitioner and left inside the uterus. Although there have been several types of IUDs, currently only two are available in the United States. Both are T-shaped and have a string at the base of the T that will extend through the cervix and lie in the vaginal canal. The copper IUD releases a small amount of copper into the uterus and may remain in your body for up to 10 years. The hormonal IUD releases a small amount of the hormone progesterone into the uterus, but must be replaced every year.
How does the copper IUD work?
It primarily prevents pregnancy by interfering with the movement of sperm thus preventing fertilization of the egg. The copper IUD prevents fertilization as well as affecting the lining of the uterus so implantation will not occur.
How effective is the copper IUD?
The IUD is extremely effective. During the first year of use, 8 out of 1000 women will become pregnant with the Copper T.
Am I a good candidate for the copper IUD?
The copper IUD is best suited for women with families who want convenient, effective, reversible contraception. It is recommended for women who have at least one child, are in a stable, mutually faithful relationship (to minimize chance of exposure to sexually transmitted diseases that might cause pelvic inflammatory disease) and have no history or suspicion of pelvic infection.
Are there any reasons why I shouldn’t use the copper IUD?
For some women, certain conditions can increase the chance of having problems with the IUD. The IUD may NOT be a good choice if you have:
- had a pelvic infection
- had an ectopic (tubal) pregnancy
- severe pain during menstrual periods
- abnormal vaginal bleeding
- multiple sexual partners or a high risk for sexually transmitted diseases
- allergy to copper
What are the common side effects of the copper IUD?
Irregular bleeding
Bleeding problems constitute one of the more common IUD complications. Some women have cramping and spotting during the first few weeks after the IUD is placed. These should disappear within a month. The IUD does cause slightly crampier and longer menstrual periods. These symptoms can be treated with Motrin or Advil.
Pelvic infection
The risk of developing a pelvic infection associated with the IUD is attributable to insertion of the device and exposure to sexually transmitted infection. The greatest risk occurs during the first few weeks following insertion. Women who have more than one sexual partner or whose partner has other sexual partners are at high risk for acquiring a sexually transmitted disease.
Expulsion
Between 2 and 10% of IUD users spontaneously expel their IUD within the first year. Expulsion, though infrequent, is more likely to occur during the first 3 months of use. An IUD expulsion can occur without a woman knowing it. Therefore, you should check regularly to make sure the “string” is still present.
What are the benefits of the copper IUD?
- Highly effective
- Easy to use
You don’t have to remember to insert it before sex or take a pill every day.
Reversible
It can be easily removed in the office if you decide to get pregnant and you do not need to wait before attempting pregnancy.
Can be used by breastfeeding women
There is no affect on lactation.
Inexpensive
After the first year of use, the annual cost for using the IUD is less expensive per year.
May be used by women who cannot use hormonal methods and causes no systemic side effects
(except in women allergic to copper or have a condition called Wilson’s disease)
Comfort
You should not be aware of the presence of the IUD. You and your partner should not be able to feel the IUD during intercourse.
When can the copper IUD be inserted?
First it must be determined that you are a good candidate for the IUD. Your doctor will take a medical history, perform a pelvic exam and obtain any appropriate lab tests.
The insertion can then be scheduled within the first 5 days of your next menstrual period; this insures that you are not pregnant at the time of insertion and the method is effective immediately for birth control.
The IUD can also be placed after giving birth, as soon as your uterus has returned to its normal pre-pregnancy state. It can be determined whether you are ready for IUD insertion at your postpartum check.
How is the copper IUD inserted?
You may be given some antibiotics to take prior to insertion to protect from infection. Also, taking 3-4 Motrin or Advil an hour prior to insertion will minimize the discomfort of the insertion.
Insertion of the IUD does not require anesthesia. Immediately before the IUD is inserted, you will be asked to sign a consent form making sure you understand everything about the insertion and a pregnancy test will be checked.
To insert the IUD, the arms of the T-shaped device are folded and the IUD is placed in a long, slender, plastic tube. The tube is then inserted into the vagina and guided through the cervix into the uterus. The IUD is then pushed out of the plastic tube into the uterus and the tube is withdrawn.
Each IUD comes with a string or “tail” made of a thin plastic thread. After insertion the thread is trimmed so that 1-2 inches hang out of the cervix inside your vagina. You will be able to tell about the placement of the IUD by the location of the string. The string will not bother you, but your partner may feel it with his penis.
If you feel discomfort, the string may be further trimmed. It is important that you check the string each month. To do this, you must insert a finger into your vagina and feel around for the string. You can do this at any time, but doing it after your menstrual period is easy to remember. If you feel the string is shorter or longer than it used to be-or if you don’t feel the string at all-call your doctor.
The IUD may have slipped out of place. Use another form of birth control until your IUD is checked.
Are there any warning signs I should look out for after the IUD is inserted?
Call your doctor if you have any of the following problems:
- Severe abdominal pain
- Pain during intercourse
- Bleeding or spotting that occurs between periods, after intercourse, or that lasts more than a few months
- Missed period or other signs of pregnancy
- Unusual vaginal discharge
- A change in length or position of the string
BIRTH CONTROL IMPLANTS
 Birth control implants are devices that go under the skin. A hormone is released that prevents pregnancy.
Birth control implants are devices that go under the skin. A hormone is released that prevents pregnancy.
DIAPHRAGM (vaginal barrier contraception)
 What is the Diaphragm?
What is the Diaphragm?
The diaphragm is a round rubber dome that fits inside a woman’s vagina and covers her cervix. It must be used with spermicide (a sperm-killing cream or jelly).
How does the Diaphragm work?
The diaphragm is a barrier method of birth control that prevents pregnancy by placing a physical and chemical “wall” between the sperm and the cervix. It must always be used with a spermicidal cream or jelly. Be sure that the jelly or cream you purchase is a spermicide containing nonoxynol-9.
How effective is the Diaphragm?
The diaphragm is NOT the most effective form of birth control. Effectiveness includes the use of spermicide. Among perfect users (women who use the diaphragm EVERY time they have sex), about 6 in 100 women (6%) is expected to become pregnant over the first year of use. Among typical users, 18 in 100 women will become pregnant over one year of use. However, using a condom along with the diaphragm will increase the effectiveness AND provide protection from sexually transmitted disease.
Am I a good candidate for the Diaphragm?
The diaphragm is worth considering if you cannot or prefer not to use hormonal birth control. You must be able to use it every time you have sex.
Are there any reasons why I shouldn’t use the Diaphragm?
The diaphragm may not be a good choice for you if you are unlikely to use it correctly every time you have sex. You may not be able to use it if you or your partner is sensitive to the chemicals used in spermicides or has a latex allergy. You may have a higher failure rate if you have intercourse three or more times per week.
What are the most common side effects of the Diaphragm?
- Increased risk of urinary tract infections
- Yeast infections and bacterial vaginosis
- Sensitivity due to latex allergy
What are the benefits of the Diaphragm?
- Almost no side effects and does not affect your hormonal pattern
- Lower risk of cervical cancer and pre-cancerous conditions of the cervix
How do I use a Diaphragm?
Wash your hands carefully with soap and water before inserting the diaphragm. Apply spermicidal cream or jelly around the rim and inside the dome of the diaphragm. You may put spermicide on both sides of the diaphragm, but make certain to apply a generous amount of spermicide on the side of the diaphragm facing or in contact with the cervix.
Squeeze the rim of the diaphragm between your fingers and insert it into your vagina. When the diaphragm is pushed up as far as it will go, the front part of the rim should be up behind a bone you can feel in front of your pelvis (the pubic bone). Tuck the front rim of the diaphragm up as far as it will comfortably go.
Check to see if your cervix is covered. To do this, reach inside and touch your cervix. The cervix feels something like the tip of your nose. After the diaphragm is in place, the cervix should be completely covered by the rubber dome.
When do I insert the Diaphragm?
The diaphragm may be placed up to 6 hours before you have sex. No matter when you insert the diaphragm, always be sure to use a spermicide. Diaphragms should not be used without this added protection.
If you have put in the diaphragm more than 2 hours before having sex, you must insert a fresh supply of spermicide into your vagina just before intercourse. To do this, insert the spermicide with an applicator while the diaphragm is in place. An applicator usually comes with the spermicide.
You must also check the position of the diaphragm and add more spermicide before each act of intercourse, no matter how closely together they occur. Do not use oil-based lubricants such as petroleum jelly; they can damage the diaphragm. Water-based lubricants such as KY jelly or Astroglide are fine.
When should I remove the Diaphragm?
The diaphragm must be left in place for 6 hours after you have sex, but should NOT be worn for more than 24 hours. To remove the diaphragm, pull gently on the front rim. Wash it with mild soap and water, rinse the soap off well (soap can harm the rubber), dry it, and put it back in its case.
When do I need to replace the Diaphragm?
The diaphragm may become discolored over time, but it can still be used unless you notice any holes in the rubber. To check for holes, hold the diaphragm up to the light and stretch the rubber gently between your fingers. Filling the diaphragm with water is another way to check for holes.
You should get a new diaphragm about every 2 years. Your diaphragm should be rechecked at your yearly exam and should be refitted if you have:
- had pelvic surgery
- been recently pregnant
- gained or lost a lot of weight
- trouble with the diaphragm slipping out of place, pain or pressure during sex
What should I do if I forgot to use the Diaphragm or placed it incorrectly?
Emergency contraception is available if you are concerned that may be pregnant. This can only be used within 72 hours of unprotected or inadequately protected intercourse. Call the office to find out more about this back-up method of birth control.
Are there any warning signs I should look out for when using a Diaphragm?
There is a slight increased risk of toxic shock syndrome in diaphragm users if it is worn for more than twenty-four hours.
Call your doctor if you have any of the following problems:
Sudden high fever, vomiting, diarrhea, dizziness, faintness, weakness, sore throat, aching muscles and joints, or a rash (like a sunburn).
 What is “tubal ligation”?
What is “tubal ligation”?